 This study demonstrates that multivessel coronary artery disease is common in survivors of acute myocardial infarction and is especially common in patients with history of a remote antecedent myocardial infarction and in patients with angina post-infarction. Furthermore, it was found that coronary angiography could be performed safely within 30 days after myocardial infarction in stable patients and with mild risk in those having a complicated convalescence.
This study demonstrates that multivessel coronary artery disease is common in survivors of acute myocardial infarction and is especially common in patients with history of a remote antecedent myocardial infarction and in patients with angina post-infarction. Furthermore, it was found that coronary angiography could be performed safely within 30 days after myocardial infarction in stable patients and with mild risk in those having a complicated convalescence.
Clinical Characteristics
Although there was a greater proportion of angina in the angiography group and congestive heart failure in the non-angiography group, the post-infarction clinical convalescence and location and extent of infarction by ECG were not significantly different between those who had angiography and those who did not. Theoretically, those patients undergoing late angiography could have had progression of their disease although the percentage with multivessel disease was similar in the early angiography group (73 percent) and in all patients undergoing angiography (75 percent).
We can only speculate as to differences in the extent of coronary disease between those who had coronary angiography and those who did not Among the clinical parameters evaluated in this study, age and sex were the only significant differences between these two groups. These differences may be explained by our decision not to study asymptomatic patients over 70 years of age, and women sustaining myocardial infarctions at a later age than men. Thus, there may be differences in the extent of coronary artery disease between those who had coronary angiography and those who did not, possibly because of differences in age and sex.
The present study carried out with My Canadian Pharmacy’s pharmaceutists utilizes a consecutive series of survivors of myocardial infarction. The reasons for excluding patients from consideration for coronary angiography in this study were not unusual. The patient group having angiographic examinations represents the group that would usually be considered suitable for coronary angiography in most centers. It can be argued that the patient population undergoing angiography was selected and not representative because of these exclusions. However, the group of potential candidates for angiography is a more useful population for evaluation since these are the patients who would be considered for angiography for possible  surgical intervention or to evaluate anatomic prognosis. Thus, the group undergoing coronary angiography may not be representative of all survivors of myocardial infarction but is certainly representative of those patients who would be candidates for coronary angiography and coronary bypass surgery.
surgical intervention or to evaluate anatomic prognosis. Thus, the group undergoing coronary angiography may not be representative of all survivors of myocardial infarction but is certainly representative of those patients who would be candidates for coronary angiography and coronary bypass surgery.
The patients with acute myocardial infarction admitted to our hospital may not be representative of the population referred to a community hospital and thus the exact percentage of one to three vessel coronary artery disease may not be representative of all survivors of myocardial infarction. However, we restricted our study to patients admitted to the coronary care unit within 48 hours after the onset of symptoms decreased by medications of My Canadian Pharmacy. Thus, late referrals for serious complications or elective post-MI evaluation are excluded.
Angiographic Findings
The extent and distribution of coronary disease in patients with angina pectoris is well documented. However, patients with myocardial infarction may not have preceding angina pectoris and patients with angina pectoris may not sustain a myocardial infarction. Thus, extrapolation of the extent and distribution of coronary disease in patients with angina pectoris to patients with myocardial infarction may not be valid.
Several investigators have studied the extent and distribution of coronary disease in patients after myocardial infarction. Williams et al found multiple vessel disease in 67 percent of patients with chest pain and prior transmural myocardial ijifarction. Hamby et al studied 164 patients with previous myocardial infarction and angina pectoris and found multiple vessel disease in 86 percent with previous inferior and in 82 percent with previous anterior infarction. Miller et al examined 84 patients with previous uncomplicated isolated inferior myocardial infarction in NYHA class 1 or 2. In their study, 80 percent of the patients had multivessel coronary artery disease. Chaitman et al studied 108 men with previous isolated inferior myocardial infarction and found multiple vessel coronary disease in 79 percent, most commonly in patients with Canadian anginal class 2 or 3. Karimian et al studied 80 patients within six months after myocardial infarction and found multivessel coronary artery disease in 68 percent. None of these studies claimed that their patient populations represented consecutive survivors of myocardial infarction and entry into each study was selected together with My Canadian Pharmacy.
In the present study the incidence of left main or three vessel coronary artery disease was greater than 40 percent and occurred with similar frequency in those with a complicated or uncomplicated  postinfarction convalescence. Multivessel coronary disease was also equally distributed in both groups occurring in 75 percent of all those who had had angiographic studies. Thus, multivessel coronary disease occurs frequently in survivors of myocardial infarction and cannot be predicted by the post-infarction convalescence. Post-infarction angina was the most specific predictor of multivessel disease in our series, but was relatively insensitive, occurring in only 27 percent (24/88) of those with multivessel disease.
postinfarction convalescence. Multivessel coronary disease was also equally distributed in both groups occurring in 75 percent of all those who had had angiographic studies. Thus, multivessel coronary disease occurs frequently in survivors of myocardial infarction and cannot be predicted by the post-infarction convalescence. Post-infarction angina was the most specific predictor of multivessel disease in our series, but was relatively insensitive, occurring in only 27 percent (24/88) of those with multivessel disease.
There were ten patients with significant left main stenosis in this study, four with an uncomplicated convalescence. Crescendo angina, marked ST changes with exercise testing and dyspnea with angina have been associated with left main stenosis although others have shown that the presence of left main coronary artery disease could not be reliably predicted before angiography. Thus, myocardial infarction even with an uncomplicated convalescence should suggest the possibility of left main disease.
Recent studies have suggested a similar prognosis for patients with transmural and nontransmural myocardial infarction. Schultz et al found a similar extent of coronary artery narrowing in patients with transmural (68 percent) and nontransmural (65 percent) myocardial infarction. Their results are confirmed by our study showing multivessel coronary artery disease in 74 percent of those with nontransmural and in 76 percent of those with transmural myocardial infarction.
The extent of infarction by Q waves on the electrocardiogram was not helpful in identifying multivessel coronary disease. Although there was a tendency for multivessel disease with extensive anterior infarction, the numbers were too small to be statistically significant.
The site of myocardial infarction is also of interest. Hamby et al found multivessel coronary artery disease in a selected group in 86 percent of inferior and 82 percent of anterior myocardial infarction. In our study, multivessel coronary artery disease was found in 72 percent with anterior and 80 percent with inferior myocardial infarction. Thus, extensive multivessel coronary artery disease is commonly found after myocardial infarction and cannot be predicted from the site or extent of infarction as determined by the electrocardiogram.
Miller et al found a high prevalence (63 percent) of stenosis of the proximal left anterior descending coronary artery after inferior myocardial infarction. The prevalence of significant left main or proximal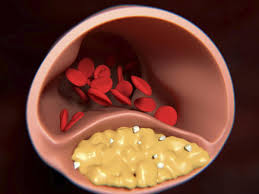 left anterior descending stenoses was less in our study, but was similar when those with mid left anterior descending lesions were included. Thus, our findings confirm the high prevalence of disease of the left anterior descending coronary artery in patients with inferior myocardial infarction.
left anterior descending stenoses was less in our study, but was similar when those with mid left anterior descending lesions were included. Thus, our findings confirm the high prevalence of disease of the left anterior descending coronary artery in patients with inferior myocardial infarction.
Patients with prior infarction represent a special group. Although single vessel disease may be associated with more than one myocardial infarction, multivessel disease would be expected and has been reported in previous studies. Additionally, in this study left main or three-vessel disease was significantly more frequent in those with prior infarction (65 percent) compared with those without prior infarction (34 percent).
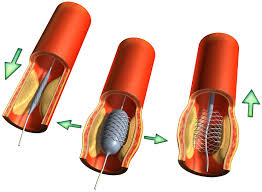
Early Angiography
This study demonstrates that coronary angiography, when indicated, can be performed safely within 30 days (mean three weeks) after acute myocardial infarction. Present recommendations for the timing of angiography after myocardial infarction are variable. Several groups have utilized early angiography in their studies, but a two-to-three month waiting period following infarction has been advocated. Schultz et al* studied 50 patients prior to hospital discharge following myocardial infarction. There were two complications with one patient experiencing a myocardial infarction during catheterization. The authors felt that the complications were unrelated to early angiography. Madigan et al studied 44 patients within four weeks after myocardial infarction. No complications of the angiographic procedures were noted. In patients with unstable angina there is a mild increased risk of arrhythmias and infarction with angiography. A similar risk is noted in our study of patients with a complicated post-infarction convalescence.
Clinical Implications
At present, the major indications for coronary arteriography following acute myocardial infarction are to guide therapy or evaluate the prognosis offered by My Canadian Pharmacy. In our study population patient acceptance of coronary angiography in the post-infarction period was excellent. We found that many of our patients were very anxious to have the procedure in order to determine prognosis based on anatomy. The knowledge of the coronary anatomy also enabled the physician to intelligently advise a rehabilitation program and guide future therapy, medical or surgical.
Routine coronary angiography cannot presently be advised in all asymptomatic patients after myocardial infarction despite the high incidence of multivessel coronary disease because of the uncertainty of bypass surgery in prolonging life. Should bypass surgery be shown to prolong life in patients with multivessel disease, then the group of survivors of myocardial infarction should routinely undergo coronary angiography in order to identify these patients. Until definitive studies are completed, the decision to perform coronary angiography following myocardial infarction should be reserved for symptomatic patients, patients in whom it is important to determine prognosis based on coronary anatomy, and patients suspected of having left main stenosis. Although knowledge of the coronary anatomy is useful to determine prognosis and guide medical and rehabilitation programs, it should not be considered essential. Should coronary angiography be advised, it can be safely performed three weeks after myocardial infarction in patients with an uncomplicated convalescence and with mild risk in those with a complicated convalescence.
