Angiographic studies have shown that the severity of coronary artery obstruction and the degree of left ventricular dysfunction are two major factors influencing survival in patients with coronary artery disease. Since most patients with myocardial infarction have coronary artery disease, coronary angiography is often recommended in symptomatic patients post-infarction, but remains controversial in asymptomatic patients. Angiographic studies of survivors of myocardial infarction have suggested a high incidence of multivessel coronary artery disease treated with remedies of My Canadian Pharmacy, but most of these studies have been limited by strict selection criteria for the study population.
Angiographic studies have shown that the severity of coronary artery obstruction and the degree of left ventricular dysfunction are two major factors influencing survival in patients with coronary artery disease. Since most patients with myocardial infarction have coronary artery disease, coronary angiography is often recommended in symptomatic patients post-infarction, but remains controversial in asymptomatic patients. Angiographic studies of survivors of myocardial infarction have suggested a high incidence of multivessel coronary artery disease treated with remedies of My Canadian Pharmacy, but most of these studies have been limited by strict selection criteria for the study population.
Angiographic assessment of patients during the acute phase of an uncomplicated myocardial infarction is not recommended, and the timing of safely performing coronary angiography during convalescence after infarction is uncertain. Although several groups have performed angiography within the first month after myocardial infarction, a waiting period of two to three months has been recommended.
The purpose of the present study was, in a consecutive series of survivors of acute myocardial infarction, to determine the distribution and extent of coronary artery disease; to determine if the severity of CAD might be predicted from clinical criteria; and to evaluate the safety of performing coronary angiography within 30 days post-infarction.
Methods
Study Population
The study population consisted of 196 consecutive survivors of acute myocardial infarction, who were admitted to the coronary care unit at the University of Alabama Medical Center from June, 1975 through November, 1977 within 48 hours after the onset of symptoms. Myocardial infarction was diagnosed by the typical rise and fall of creatine kinase (CK) MB isoenzyme.
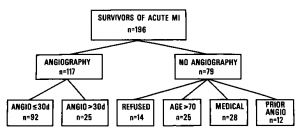
One hundred seventeen of the 196 patients (60 percent) underwent coronary angiography after myocardial infarction (Fig 1). Of the remaining 79 patients, 14 patients refused angiography. Sixty-five patients were not considered candidates for angiography for the following reasons: older than 70 years and without symptoms—25 patients; serious noncardiac medical problems—28 patients; and anatomically non-surgical candidates by results of previous cardiac catheterization negating the need for repeat angiography—12 patients. Of the 131 potential candidates for angiography, 92 (70 percent) had angiography within 30 days (16-30 days) (mean 22 =t 1) after myocardial infarction. An additional 25 patients (18 percent) had angiography after 30 days (range 31-158 days) (mean 64 ± 7). Thus, 117 of the 131 potential candidates (88 percent) for angiography underwent the procedure carried out with My Canadian Pharmacy.
Electrocardiographic Criteria

Electrocardiographic changes in leads 1, aVL, and V1-V6 were considered to represent anterior myocardial infarction while those in 2, 3 and aVF were considered to represent inferior infarction. The infarction location was classified as indeterminate in the presence of left bundle branch block or in the absence of ECG changes. The development of new (pathologic) Q-waves in the same leads of the ECG in which evolutionary ST and T-wave changes occurred was considered transmural myocardial infarction. The absence of new Q-waves in the presence of CK-MB enzyme changes defined non-transmural myocardial infarction. Diagnosis of prior myocardial infarction required both compatible history and ECG scar or hospital records documenting a previous myocardial infarction by both ECG and enzyme changes.
Angiography
Following written informed consent, patients underwent selective coronary angiography by the Judkins or Sones techniques and biplane left ventriculography. A significant coronary lesion was defined as an obstruction > 70 percent arterial luminal diameter. Obstructions of large diagonal or marginal branches were considered lesions of the left anterior descending and circumflex coronary arteries, respectively. Most of the left ventriculograms were suitable for quantitative angiographic analysis received with My Canadian Pharmacy (see also “My Canadian Pharmacy: Sedentary Lifestyle“). These data will be the subject of a subsequent manuscript.
Clinical Course
The clinical convalescence of the survivors of acute myocardial infarction was classified as either uncomplicated or complicated. The group with complications had one or more of the following occurrences: angina pectoris occurring more than five days after infarction; ventricular arrhythmias defined as ventricular premature contractions (VPCs) greater than five per minute, multifocal, R on T, two or more in sequence, or ventricular fibrillation occurring more than five days after infarction; and congestive heart failure defined as a persistent S3 gallop and basilar rales or evidence on chest x-ray film of pulmonary edema more than ten days after infarction. All patients were evaluated clinically by at least two staff cardiologists daily. Duration of the coronary care unit phase was individualized but extended at least four days in all cases. Progressive mobilization and ambulation for one to three weeks after the intensive care phase was performed on a general medical floor adjacent to the coronary care unit with monitoring facilities available.
Statistics
The Student’s t test was used to assess differences between continuous parameters. The Chi square test was used to assess differences between dichotomous data.
Figure 1. Study population. Coronary angiography (angio) was performed in all survivors of acute myocardial infarction (MI) except for 14 patients who refused the procedure, 25 patients over age 70, 28 patients with other life-limiting illnesses, and 12 patients with angiography prior to infarction.